Vaginoplasty is a complex surgical procedure involving reconstruction or creation of the vaginal canal and external genitalia. Whether performed as part of gender-affirming surgery (MTF) or to restore function and aesthetics in cisgender women, one of the most commonly asked—and medically significant—questions is: “When can you have sex after vaginoplasty?”

This article provides a science-based timeline for recovery, explains what happens during healing, outlines risks of premature sexual activity, and answers critical questions like “how long after vaginoplasty can you have sex?” and “how does sex feel after vaginoplasty?”
Understanding Vaginoplasty and the Healing Process
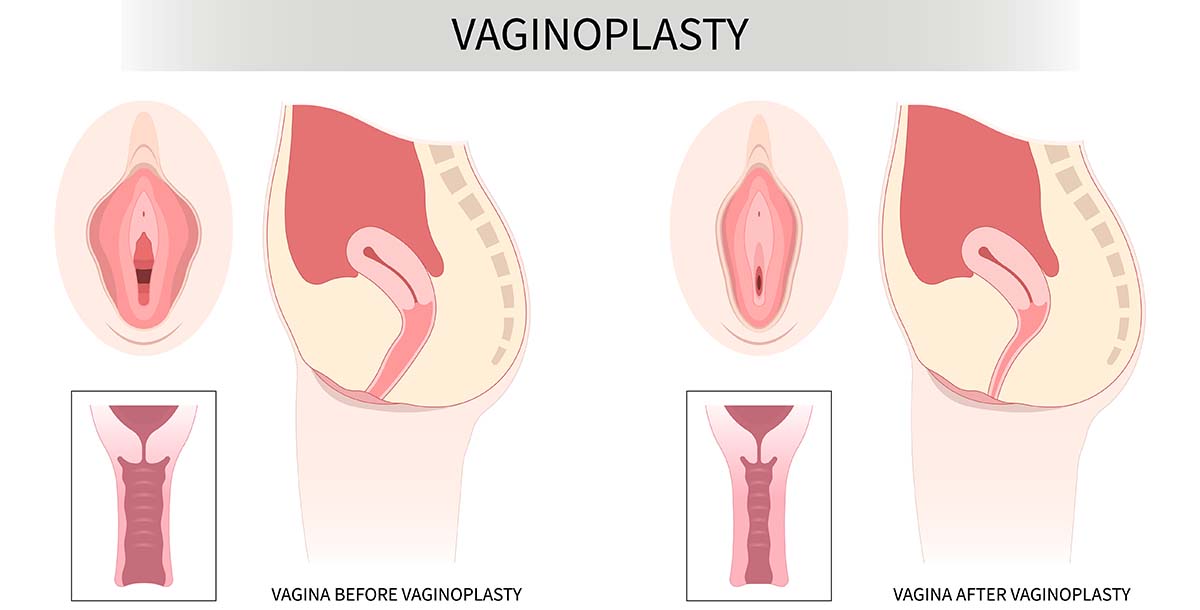
Vaginoplasty typically involves dissection and formation of a neovaginal canal, use of penile or scrotal skin grafts (in MTF procedures), and creation or reshaping of the vulva and clitoral hood. In cisgender women, it may include tightening of the vaginal walls, perineorrhaphy, or reconstruction after trauma or childbirth.

The healing process occurs in phases:
- Hemostasis and Inflammation (Days 0–7): Swelling, bruising, and initial wound healing.
- Proliferation (Weeks 1–4): Epithelialization and collagen deposition.
- Maturation and Remodeling (Weeks 6–12+): Scar softening and tissue stabilization.
For most patients, the vagina after vaginoplasty requires months to become functionally resilient and pain-free, particularly for penetrative intercourse.
How Long After Vaginoplasty Can You Have Sex?
The short answer: Most surgeons recommend waiting at least 6–8 weeks post-surgery before engaging in penetrative sex, but this is not universal. Several factors influence the timeline, including:
- Surgical technique and graft type
- Whether the procedure was primary or a revision
- Individual healing rate
- Dilator compliance (especially in sex after vaginoplasty MTF cases)
- Presence of complications (e.g., granulation tissue, stenosis)
Surgeons usually clear patients for intercourse only after verifying that the vaginoplasty is fully healed, there is no infection or bleeding, and dilator use is comfortable.
Clinical consensus suggests that penetrative intercourse before 6 weeks risks dehiscence, infection, or long-term scarring, and may compromise both aesthetics and function [1].
Signs Your Body Is Ready for Sex After Vaginoplasty
While a surgeon’s clearance is the gold standard, patients can monitor several indicators that the body is ready for intercourse:
- No signs of infection (discharge, redness, odor)
- Absence of active bleeding or open wounds
- Completion of initial dilator therapy without discomfort
- Restored elasticity and moisture (natural or estrogen-supported)
- Emotional readiness and absence of pain during touch
Especially in sex after vaginal rejuvenation or post-menopausal repairs, lubrication and estrogen levels should be optimized beforehand.
Why Having Sex Too Early Can Be Dangerous

Premature sexual activity may cause:
- Wound dehiscence: Reopening of the surgical site
- Infections: Bacterial vaginitis or urinary tract infections
- Vaginal stenosis: Scar tissue formation causing narrowing
- Loss of depth or sensitivity in the vagina after vaginoplasty
These complications can lead to corrective surgery, prolonged pain, or reduced sexual satisfaction. Healing timelines should never be rushed for short-term gratification.
A 2018 study in Plastic and Reconstructive Surgery – Global Open emphasized the need for a cautious, patient-specific timeline to protect long-term outcomes [2].
How Does Sex Feel After Vaginoplasty?
Many patients report improved sensation and confidence once fully healed. However, expectations must be grounded in medical reality.

In sex after vaginoplasty MTF, patients may experience:
- Positive erogenous sensation from the neoclitoris
- Some tightness or discomfort initially
- Variable vaginal lubrication, often requiring external aids
- Emotional euphoria tied to gender affirmation
In cosmetic/reconstructive cases, patients often notice:
- Improved tone and friction
- Reduced laxity and increased partner satisfaction
- Better control of urinary or pelvic floor symptoms
A fully healed vaginoplasty generally allows for satisfying intercourse, provided emotional and psychological readiness are in place.
Tips for a Safe Return to Intercourse
Once cleared, consider the following for a smoother transition:
- Use ample lubrication, preferably water-based or silicone, especially in hypoestrogenic states.
- Start slowly with digital or dilator-assisted exploration before partner penetration.
- Choose positions that reduce pressure on healing tissue.
- Communicate with your partner to avoid anxiety or overexertion.
- Consider pelvic floor therapy if tension or pain persists.
In sex after vaginoplasty, patience, gentleness, and awareness of body signals are essential.
What If Sex Is Painful After Vaginoplasty?
Pain during intercourse, or dyspareunia, can persist for months in some patients and must be addressed promptly.
Potential causes include:
- Scar contracture
- Inadequate depth or dilation
- Vaginal dryness or low estrogen
- Emotional trauma or fear
Management may involve:
- Topical estrogen (especially post-menopause)
- Vaginal moisturizers and lubricants
- Ongoing dilator therapy
- Referral to a pelvic floor physical therapist or sex therapist
According to the World Professional Association for Transgender Health (WPATH), up to 15% of patients undergoing MTF vaginoplasty may report initial sexual discomfort, which often improves with therapy and time [3].
Professional Follow-Up Is Essential

Even if the vaginoplasty is fully healed externally, only your surgeon can assess internal scarring, vaginal depth, and readiness for sexual activity. A proper post-operative exam typically includes:
- Vaginal inspection
- Palpation of surgical scars
- Assessment of elasticity and sensitivity
- Counseling for partner-based sexual re-entry
Never rely solely on internet advice or anecdotal reports. Always seek expert input.
Empowered Intimacy Begins with Healing
Returning to sex after surgery can be deeply affirming—but only if done with care. Knowing how long after vaginoplasty can you have sex, what signs to watch for, and what support systems exist can dramatically influence your outcome.
For many patients, sex after vaginoplasty is not just about pleasure—it’s about reclaiming identity, functionality, and intimacy on their own terms.
Reclaim Your Confidence with Expert Support
Navigating the timeline for sex after vaginoplasty isn’t just about counting weeks—it’s about restoring full confidence in your body and intimacy. Whether you’re seeking guidance on how does sex feel after vaginoplasty or wondering if you have a fully healed vaginoplasty, your care team is your best ally.
If you have questions or concerns, schedule a follow-up visit with your surgeon or consult a pelvic floor specialist. True healing is both physical and emotional, and worth waiting for.
References
- van der Sluis, W. B., et al. (2016). Surgical outcome and patient satisfaction of penile inversion vaginoplasty in transgender women. Journal of Sexual Medicine, 13(10), 1645–1651.
- Levitt, J. O., et al. (2018). Postoperative care in gender-confirming surgery. Plastic and Reconstructive Surgery – Global Open, 6(10), e1950.
- WPATH. (2022). Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. International Journal of Transgender Health, 23(S1), S1–S259.
- Wittenberg, M., et al. (2021). Pain after vaginoplasty: Etiology and treatment. Obstetrics & Gynecology Clinics, 48(4), 819–832.
- Safer, J. D., & Tangpricha, V. (2019). Care of the transgender patient. Annals of Internal Medicine, 171(7), ITC49–ITC64.






